Clomiphene Versus Letrozole: Which Works Better?
How Each Medication Works Inside the Body
Teh two drugs start with distinct signals: clomiphene binds estrogen receptors in the hypothalamus and pituitary, tricking the brain into sensing low estrogen and boosting GnRH, FSH and LH to encourage follicle growth and ovulation. Letrozole, an aromatase inhibitor, lowers systemic estrogen synthesis so negative feedback loosens and FSH rises, often producing a shorter, more physiologic estrogen exposure during follicular development.
Clinically the differences matter: clomiphene’s longer receptor effect can thin endometrium and alter cervical mucus, sometimes reducing implantation potential, while letrozole generally preserves endometrial lining and may yield better quality follicles. Pharmacokinetics, timing, previous responses and patient enviroment shape choice, so clinicians tailor dose, cycle monitoring and follow up to balance conception chances with safety. Individual fertility history, BMI, ovulatory reserve markers and coexisting conditions guide selection and may influence duration, monitoring frequency and eventual live birth outcomes significantly.
Comparing Effectiveness: Pregnancy and Ovulation Rates

Patients often tell stories of cycles finally responding after months of frustration, and the data helps explain why. Ovulation rates with clomiphene are generally respectable — many studies report 60–80% per cycle in responsive women — but ovulation alone doesn't ensure pregnancy. Letrozole in several trials showed higher live-birth rates for women with PCOS, suggesting better endometrial and luteal conditions.
Clinicians weigh numbers alongside personal context: age, BMI, prior miscarriages, and how many cycles have been attempted. Teh gap between ovulation and live birth rates reminds patients that monitoring, timing and follow-up IUI or IVF choices matter. For some, clomiphene remains a good first step; for others, letrozole provides a statistically meaningful advantage in practice.
Side Effects and Long Term Safety Considerations
Patients remember the week of treatment by its side effects: hot flashes, bloating, mood swings and, with clomiphene, Occassionally visual blurring that should prompt review. Letrozole tends to cause fatigue, headaches and musculoskeletal aches rather than thicker endometrium, so cervical response differs. Both drugs can produce multiple follicles, raising OHSS and multiple pregnancy risk.
Long-term data from infertility cohorts are reassuring: short courses have not shown increased congenital anomalies, and bone effects are negligible for brief cycles, though extended aromatase inhibition might be a consideration in other contexts. Clinicians recomend limiting cycles, regularly monitoring ovary size and endometrium, and tailoring choice to patient history — that balance of benefits and risks is the pragmatic guide.
Who Benefits Most: Matching Patient Profiles

Imagine a woman in her early thirties with irregular cycles and a longed-for pregnancy: clomiphene often becomes the first stop in her journey because it stimulates ovulation reliably, is well-studied, and is easy to monitor. For those with polycystic ovary syndrome or unexplained infertility, clinicians frequently start with clomiphene, adjusting dose and adding IUI when appropriate; younger patients with normal ovarian reserve tend to respond best and require fewer invasive options.
Conversely, older patients or those with obesity, diminished ovarian reserve, or prior clomiphene failure may be guided toward aromatase inhibitors or IVF, since letrozole can outperform clomiphene in some PCOS populations. Shared decision-making should weigh side effects, prior treatment history, and cost. Clinicians Acommodate individual goals, and patients should expect careful cycle tracking and flexibility — Occassionally simple protocol changes improve chances and seek prompt follow-up for any concerns.
Practical Tips for Using Each Drug Effectively
When starting ovulation therapy, clear timing and tracking help outcomes. For clomiphene, take pills early in cycle and chart basal temperature, ovulation predictor kits, and cervical mucus to spot fertile window. Speak with your clinician about dose adjustments and when to transition to injectables if cycles remain anovulatory.
Letrozole requires similar monitoring but may need different timing and shorter courses; discuss side effect management and contraception after treatment. Keep expectations realistic, aquire reliable support, and log responses so both you and your provider can refine strategy for the next cycle.
Cost, Accessibility, and Real World Treatment Experiences
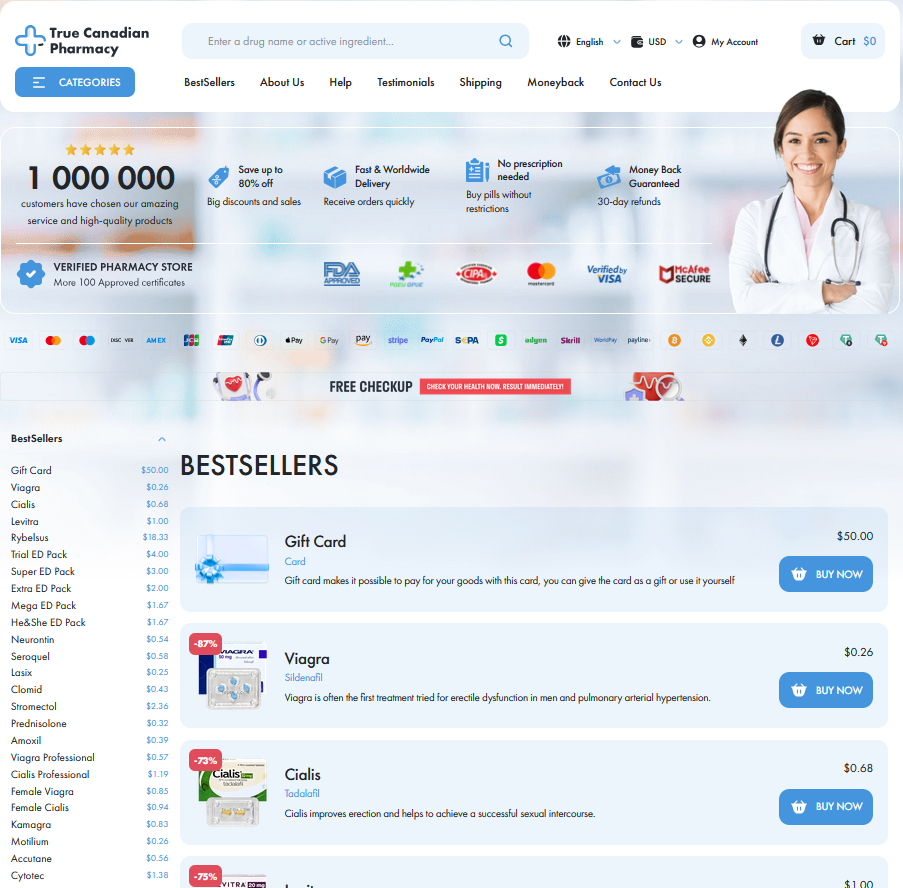
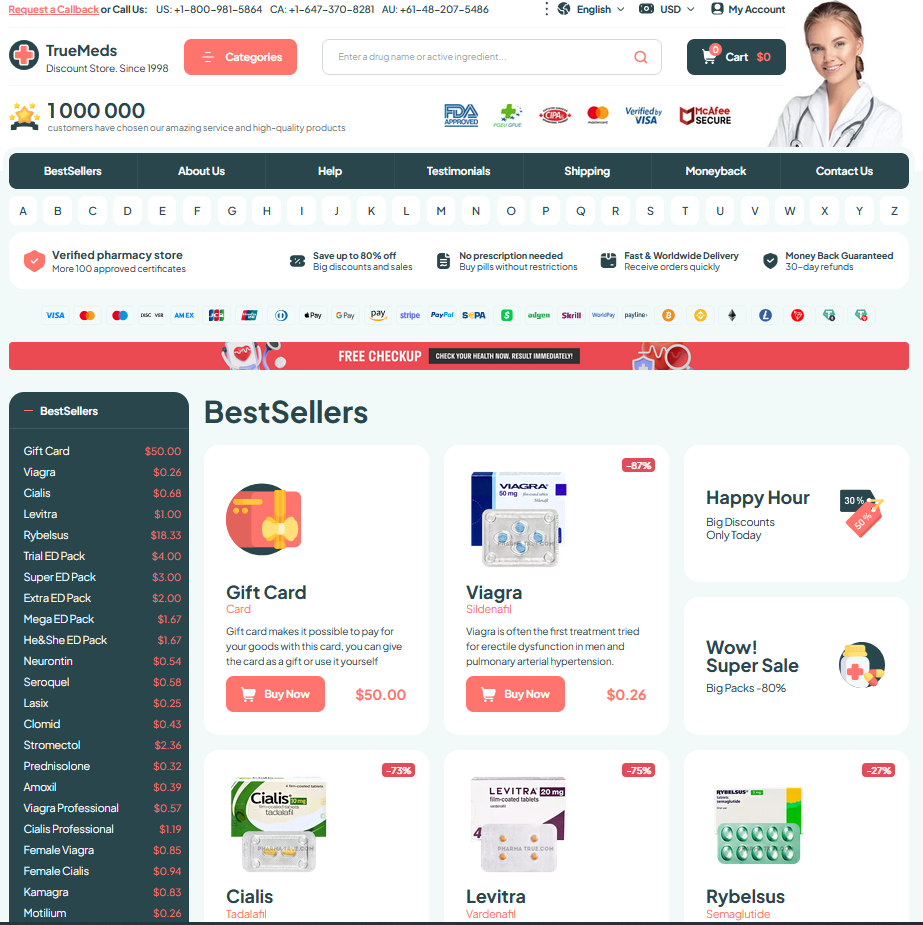
Patients weigh price and clinic access when choosing ovulation meds; generic clomiphene is usually cheaper and stocked widely, while alternatives can be pricier or restricted. In many clinics people start locally, but monitoring intensity, travel for scans, and extra fees for labs differ, so budgets and schedules shape decisions.
Forum reports and clinic notes show mixed journeys: some conceive quickly, others switch after side effects or poor response. Clinicians tailor doses, track outcomes, and discuss likely expenses so patients set realistic expectations and recieve timely follow-up with clear next steps. StatPearls: Clomiphene citrate NEJM: Letrozole vs Clomiphene